From First Use to Crisis: How Drugs Hijack the Brain and Mental Health

November 24, 2025
Key Takeaways
- Drug use lies on a continuum from casual to compulsive
- Addiction reshapes brain pathways, not just behavior
- Mental illness and substance use reinforce one another
- Cannabis and stimulants can trigger psychotic symptoms
- Recovery means restoring both the brain and behavior
- Courts that recognize this science improve outcomes
The Story Behind Every Relapse
Most people entering a treatment court didn’t begin with an addiction—they began with use.
A drink at a party.
A pain pill after surgery.
A joint to “take the edge off.”
Over time, that simple act of relief or curiosity can evolve into dependence and disease. Understanding how this progression unfolds is critical for any court or clinician (or any parent, for that matter) trying to balance accountability with compassion.
Addiction isn’t a failure of will. It’s a predictable sequence of biological, psychological, and social changes that hijack the brain.
When it comes to drug monitoring, we’re not just addressing behavior but treating changes in the brain.
The Use Continuum: From Experimentation to Dependence
Substance use exists on a spectrum.
At one end is experimental use—occasional and often social.
At the other is addiction, where control is lost, and consequences multiply.
Between those points lie stages that every court participant has traveled.
| Stage | Description | Brain and Behavior Impact |
|---|---|---|
| Experimentation | Curiosity, social use | Mild dopamine activation, no major adaptation |
| Regular Use | Weekend or coping use | Early tolerance, reinforcement of the reward loop |
| Risky Use | Increased frequency, rule-breaking | Impaired judgment, reduced inhibition |
| Dependence | Withdrawal, cravings | Brain chemistry altered. The need for the drug replaces logical choice |
| Addiction | Compulsion despite harm | Structural brain changes occur with increased loss of control |
With repetition, the brain’s reward system recalibrates. Dopamine surges that, at one point, felt pleasurable now feel normal. Without the substance, the person feels anxious, restless, or numb.
At this stage, “choice” becomes less about desire and more about survival. So, relapse isn’t a moral failure but the brain seeking equilibrium. For courts, this understanding matters. It reframes relapse as data, not defiance. Every positive test is an opportunity to assess triggers, treatment, and progress rather than to assume noncompliance.
The Brain on Drugs: How Addiction Rewrites Control
The brain is designed for reward. Food, connection, and achievement release dopamine—a signal of pleasure and motivation. Drugs hijack this process.
Cocaine, methamphetamine, opioids, and cannabis all flood the reward pathway with dopamine. Over time, natural rewards like family, work, and hobbies can stop registering. The user chases the chemical shortcut, even as clear and logical consequences multiply in their life.
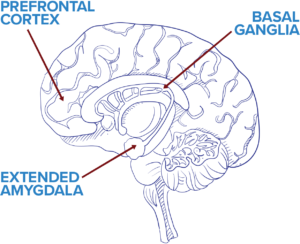
Three Critical Brain Regions Affected
- Basal Ganglia (Reward Center): learns that a drug equals pleasure, reinforcing repetition.
- Amygdala (Emotion Center): heightens stress when drugs are absent, fueling cravings.
- Prefrontal Cortex (Decision Center): weakens, making impulse control and judgment harder.
These neuroadaptations explain why addicted individuals appear irrational. The brain isn’t broken—it’s been rewired for survival around the substance. Repeated exposure changes both structure and chemistry. In fact, MRI studies show reduced gray matter in regions of the brain responsible for decision-making and emotional regulation. When the brain says “need” instead of “want,” recovery requires time and structure to rebuild those pathways. Put another way: addiction changes the brain’s operating system, and treatment is the necessary “reboot.”
When Substance Use Triggers Mental Illness
For some, drug use does more than alter mood—it triggers full psychiatric symptoms. This is especially true for high-potency cannabis, stimulants, and hallucinogens.
Cannabis-Induced Psychosis
Modern cannabis strains can exceed 20–30% THC. At those concentrations, the brain’s endocannabinoid system can become overstimulated.
In vulnerable individuals, particularly adolescents and those with family histories of psychosis, this can lead to hallucinations, paranoia, or delusional thinking. Symptoms may resolve with abstinence, but repeated episodes increase the likelihood of chronic psychotic disorders later in life.
Courts should note that psychosis from cannabis or methamphetamine can impair reality testing and competency, affecting compliance and treatment outcomes.
Stimulant-Induced Psychosis
Methamphetamine and cocaine produce similar effects. Extended binges raise dopamine to toxic levels, leading to agitation, insomnia, and paranoia. Even after detox, symptoms can persist for weeks as the brain recalibrates.
Understanding these reactions prevents mislabeling participants as defiant or dishonest when they may be experiencing acute psychiatric distress.
Co-Occurring Disorders: When the Mind and Brain Turn on Each Other
Addiction rarely travels alone. Roughly half of those with substance-use disorders also live with depression, anxiety, PTSD, or another mental-health condition.
These are called co-occurring disorders. Essentially, two illnesses that feed one another.
The Cycle
- A person with untreated trauma or depression uses drugs to cope.
- The brain’s chemistry shifts, worsening anxiety or mood instability.
- The new emotional distress drives further use.
This creates a self-perpetuating loop where each disorder reinforces the other. It also magnifies risks for suicide.
According to the CDC, individuals with both mental-health and substance-use disorders are five times more likely to attempt suicide than those with either condition alone.
Courts see this reality every day.
A participant’s relapse may not be about craving but about untreated depression. Without integrated care, each response becomes a temporary patch rather than a long-term solution. Key principle: treating only the drug use or only the mental illness guarantees relapse. Success requires coordination between court staff, clinicians, and monitoring teams.
Why Understanding the Brain Matters in Court and Treatment
Every drug court balances two responsibilities: accountability and recovery.
Neuroscience helps unite them.
When judges and probation officers understand how addiction rewires decision-making, sanctions can become corrective rather than purely punitive.
When clinicians recognize how trauma and mental illness fuel relapse, they can tailor interventions that actually stick and lead to lasting behavior change.
Continuous monitoring tools, such as the PharmChek® Sweat Patch, make that science actionable. Because the patch collects evidence of drug use over 7–10 days, it provides a continuous record that is far more reliable than a single urine test. And every presumptive positive using PharmChek® is automatically confirmed by LC-MS/MS, the platinum standard in forensic toxicology. That dual process of screening and confirming virtually eliminates false positives and protects both participants and programs from legal challenge. Courts nationwide have upheld PharmChek® results when supported by clear documentation and scientific testimony.
When due process and reliable data intersect, justice and treatment work hand in hand.
From Accountability to Recovery: Healing the Brain Takes Time
The good news: the brain can heal.
Neuroplasticity, or the brain’s ability to form new connections, allows recovery to rebuild lost function. But healing takes structure, consistency, and time.
Early in sobriety, judgment and impulse control are still impaired. That’s why external accountability matters. Continuous monitoring, therapy, and stable support create the repetition needed for new pathways to form.
Courts that blend evidence-based supervision with treatment are not “soft on crime,” they are hard on relapse, soft on shame, and committed to outcomes that last.
Every confirmed test, every documented sanction, every fair hearing helps restore the neural pathways of choice.
FAQs
What causes drug-induced psychosis?
High doses or prolonged use of stimulants, hallucinogens, or high-THC cannabis can disrupt dopamine signaling and trigger psychotic symptoms.
Can the brain heal from addiction?
Yes. With sustained abstinence, counseling, and structure, neural pathways can recover. This process may take months or years.
What are co-occurring disorders?
They are conditions in which a mental-health disorder and a substance-use disorder occur together, each worsening the other.
Why do courts use continuous monitoring?
Courts use PharmChek® for continuous monitoring because it provides accountability without intrusion, better relapse detection, scientifically defensible results, and a consistent deterrent effect that strengthens both fairness and long-term rehabilitation outcomes.
How can treatment courts balance accountability and compassion?
By pairing reliable testing and due process with trauma-informed care and individualized treatment plans.
Final Thoughts
Drug use, addiction, and mental illness form a single continuum, not separate problems to be treated in isolation. Understanding the brain science behind that continuum transforms how courts interpret relapse, design sanctions, and measure progress.
Every fair, evidence-based decision helps not only rebuild a life but also rewire a brain.